WHO IS A CANDIDATE FOR REVERSE TOTAL SHOULDER ARTHROPLASTY?
The most common indication for a reverse total shoulder arthroplasty (RTSA) is rotator cuff arthropathy (shoulder arthritis + a large rotator cuff tear). Significant or massive rotator cuff tears that are left untreated can result in the humeral head migrating upwards, resulting in loss of normal joint space. This loss of space results in deterioration of the cartilage of the shoulder joint, causing significant pain and loss of normal shoulder function. Other indications for reverse total shoulder arthroplasty include severe fractures of the proximal humerus (arm bone).
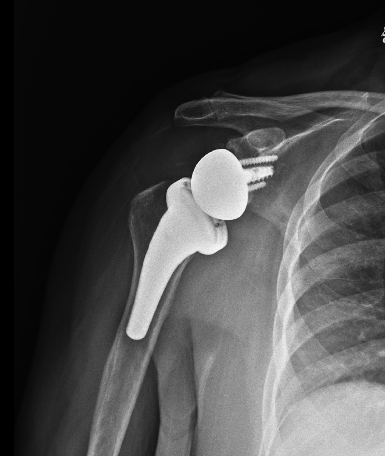
X-Ray of Reverse Total Shoulder Arthroplasty
ABOUT RTSA SURGERY
In Reverse Total Shoulder Arthroplasty, an open incision is made over the front of the shoulder. The muscles are split to allow the surgeon access to the shoulder joint. The ball and socket are resurfaced with metal and plastic components specifically sized to your shoulder. In a Reverse Total Shoulder Replacement, the ball and socket are anatomically reversed (the ball is placed over the glenoid, and the socket is placed on the humerus). This allows the deltoid muscle to compensate for rotator cuff deficiency and allow patients to lift their arm.
Reverse Total Shoulder Arthroplasty may be performed under General Anesthesia with an option for nerve block. It is usually performed outpatient, which means the patient goes home the same day or has a 23-hour overnight stay.

Example of Proximal Humerus Fracture Requiring RTSA
WHAT TO EXPECT AFTER SURGERY
It is reasonable to expect regaining functional motion after surgery, i.e. reaching overhead, reaching out the side, and to your low back. Pverall strength will return by 6 months but very heavy lifting should be avoided, if possible. Pain relief is one of the biggest benefits from RTSA.
RECOVERY PROTOCOLS OF RTSA
To speed healing, Sano Orthopedic surgeons will recommend some restrictions and rehab, including:
- Following RTSA, you will use a sling for comfort for 2 weeks.
- Formal physical therapy is recommended to begin at 2 weeks post-op. Dr. Daggett’s patients will begin passive range of motion exercises (JPL program) few days after surgery.
- Restrictions include no pushing from a seated position or lifting anything heavier than a coffee cup for 6-8 weeks post-op.
- Many patients feel most comfortable sleeping propped up in a recliner, couch, or wedged pillow after surgery.
- Patients need to keep the wound clean and dry for 10-14 days following surgery to allow the wound to heal. Use of water-proof bandages or saran wrap while showering is encouraged.
- The full release is anticipated at approximately 4-6 months post-op.